For Telemonitoring Providers
Integration
Documentation
Global Architecture
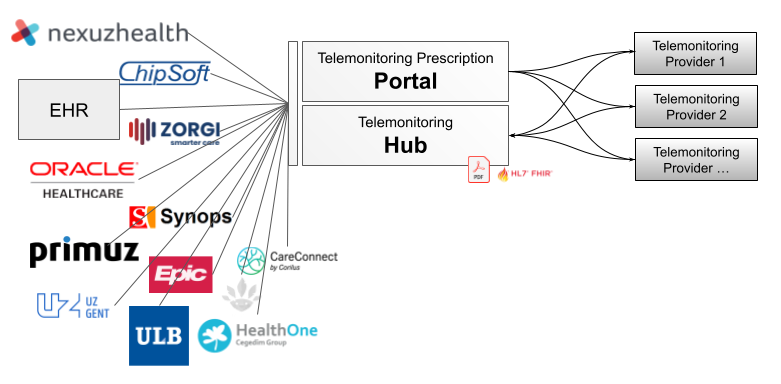
Context Integration
Context Integration is used to send EHR information to the Telemonitoring Provider.
This is done through the Telemonitoring Prescription Portal and will send a prescription request to the provider via a JSON REST call.
The Telemonitoring Prescription Portal is used directly by the HCP via a User Interface.
Security
The communication between Portal and Provider happens through HTTPS calls. These calls are protected with authentication headers chosen by the Telemonitoring Provider. The Telemonitoring Provider chooses which fixed headers are set by the Provider and which are configurable by the hospital. This way a hospital can have multiple instances of Telemonitoring Provider applications, defined by different custom headers.
The Prescription Request
The Prescription Request is triggered when a HCP clicks on the ‘prescribe’-button.
A HTTPS POST request will be triggered and will contain at least the following default content
{
"telemonitoringId": "xxx",
"patientId": "yyy",
"prescriber": {
"id": "zzz",
}
}telemonitoringId : This ID is unique within the Telemonitoring Portal and is needed if you want to attach results of the Telemonitoring Service back to the EHR.
patientId : A unique patient identifier defined by the hospital. Ideally this is a pseudonymized ID only known by the hospital, who can map this back to the patient.
prescriber > id : A unique hospital identifier. This is globally unique.
Next to this type of data other data can be requested as well.
This is the current, non exhaustive list of data you can receive. Note that more data can be requested and we’ll continue working with EHR’s to expose this data if the Telemonitoring Provider needs it to run successful Telemonitoring Sessions.
| patientId | Unique pseudonymized identifier of the patient |
| patient > citizenId | SSIN of the patient |
| patient > firstName | Firstname of the patient |
| patient > secondName | Secondname of the patient |
| patient > lastName | Lastname of the patient |
| patient > email | Email of the patient |
| patient > birthDate | Birthdate of the patient |
| patient > gender | Gender of the patient |
| patient > language | Language of the patient (2 characters) |
| patient > nationality | Nationality of the patient |
| patient > street | Street of the patient |
| patient > number | Street number of the patient |
| patient > bus | Street bus of the patient |
| patient > postalCode | Postal Code of the patient |
| patient > city | City of the patient |
| patient > country | Country of the patient |
| patient > tel | Deprecated – replaced by phoneNumber |
| patient > phoneNumber | Phone number of the patient |
| patient > mobilePhoneNumber | Mobile phone number of the patient |
| prescribingHcp > id | Deprecated – RIZIV number of the prescribing HCP |
| prescribingHcp > healthProviderId | RIZIV number of the prescribing HCP |
| prescribingHcp > citizenId | SSIN of the prescribing HCP |
| prescribingHcp > firstName | First Name of the prescribing HCP |
| prescribingHcp > lastName | Last Name of the prescribing HCP |
| responsibleHcp > id | Deprecated – RIZIV number of the responsible HCP |
| responsibleHcp > healthProviderId | RIZIV number of the responsible HCP |
| responsibleHcp > citizenId | SSIN of the responsible HCP |
| responsibleHcp > firstName | First Name of the responsible HCP |
| responsibleHcp > lastName | Last Name of the responsible HCP |
| generalPractitioner > healthProviderId | RIZIV number of the GP |
| generalPractitioner > citizenId | SSIN of the GP |
| generalPractitioner > firstName | First Name of the GP |
| generalPractitioner > lastName | Last Name of the GP |
The following fields are currently being investigated to add :
| surgery > procedure > id | procedure code |
| surgery > procedure > description | procedure humanly readable description |
| surgery > procedure > startDate | start date of the procedure |
| surgery > procedure > surgeon > id | RIZIV number of the surgeon |
| surgery > procedure > surgeon > firstName | First Name of the surgeon |
| surgery > procedure > surgeon > lastName | Last Name of the surgeon |
| surgery > procedure > laterality | Laterality within the procedure |
When receiving this request as a Telemonitoring Provider you have three options :
Option 1 : You have enough information and can confirm the request
in this case you return a status code 200, with an empty body
Option 2 : You need more information and can not confirm the request (yet)
You return a status code 200, body should contain a URI where you can fill in the missing information : { url : <https://...>}
Option 3 : You can’t confirm the request (because of any reason)
If you do not want to accept the request you should return a different status code, like 401 or 404.
You can include a message in the body to explain the reasoning : { message : 'DPA has not been signed yet' }
The Prescription Request End-Point
The above POST call will be send to a pre-defined end-point at the Providers side. If the Telemonitoring Provider has separate end-points per Prescriber, for example because the service of the Telemonitoring Provider is hosted within the prescribers environment, this is also supported by the Telemonitoring Hub. In that case the endpoint will be configured with the unique configuration enabling a Telemonitoring Provider for a specific Prescriber.
As mentioned above in the Security section, each call towards the Telemonitoring Provider can be secured with extra headers as defined by the Telemonitoring Provider. These specific headers can either be configured to be the same for each call, regardless of the Prescriber, or be uniquely configured per Prescriber.
Outcome Integration
Authorization
All API calls towards the Telemonitoring HUB require an Authorization Header. The Telemonitoring Provider will have to request a valid access_token based on the provided client and secret.
| HTTPS | POST | https://api.telemonitoring-prescription.com/auth/providers |
| HEADER | Authorization | Base64 encoded client:secret (provider specific) |
Example Response :
{
"access_token":"eyJhbGciOiJIU...",
"token_type":"bearer",
"expires_in":3600
}The client and secret are specific to a Telemonitoring Provider. Requesting a client ID and secret can be done via support@telemonitoring-prescription.com, check out the I want to get started section at the bottom of this page.
Status Update
EHR’s can be kept up to date with the data you provide as a Telemonitoring Provider. This is done by informing the Telemonitoring HUB with the needed information.
Keep in mind that informing the Telemonitoring HUB is only possible with the Telemonitoring ID. This ID is received during the request through Context Integration.
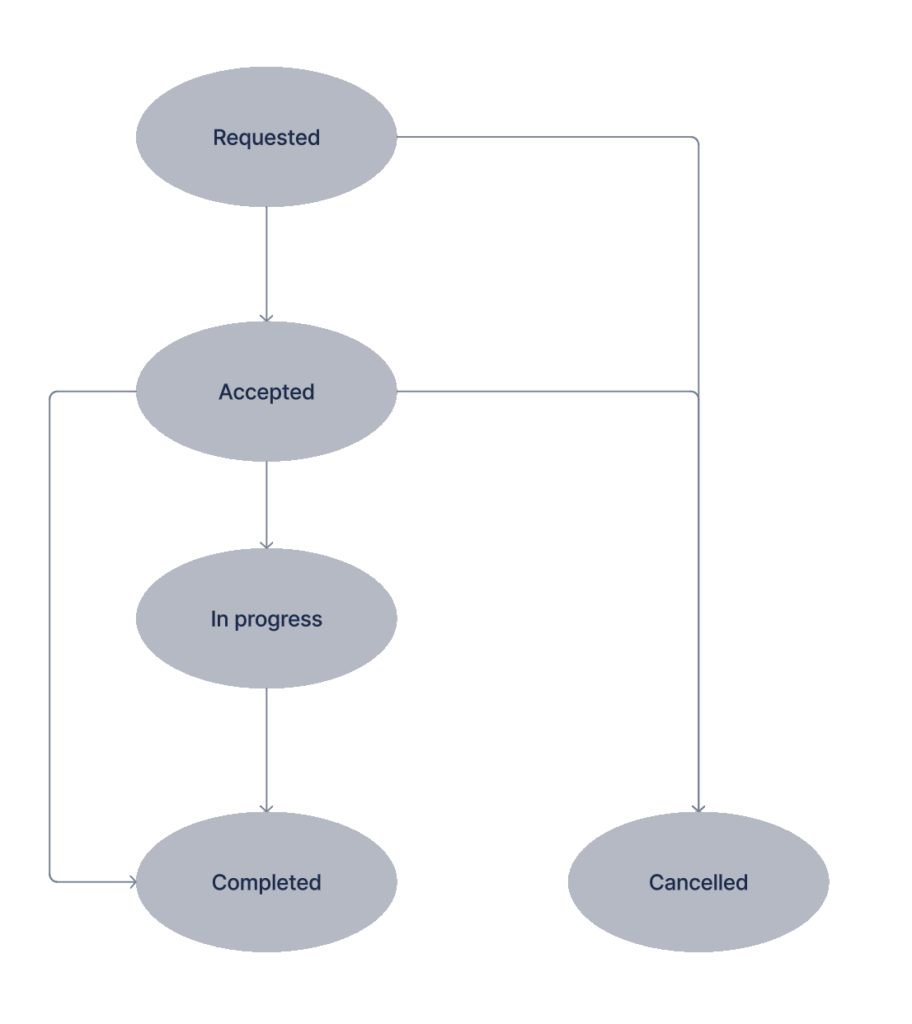
A Telemonitoring Session always has a status. The diagram below shows the possible statuses and the possible. transitions between those statuses. As Telemonitoring Provider you are the owner of the status of each session. An HCP can request a status change though the supported actions (see later section).
Carepath HL7
During a status update call it’s possible as a Telemonitoring provider to inform the EHR about the carepath for which the Telemonitoring Prescription has been created via the carepath property. This carepath property can be passed along with any status update towards the Telemonitoring HUB and will be persisted with the corresponding telemonitoringId. This means that as a Telemonitoring Provider you only have to pass the carepath once or you can also decide to pass it towards the Telemonitoring HUB with each update. The carepath is added by the provider when there is a link to a validated HL7 carepath. This link refers to to the HL7 implementation Guide.
Example carepath for Heartfailure can be found here (Telemonitoring Hub Identifier): https://build.fhir.org/ig/hl7-be/patient-monitoring/branches/main/heartfailure.html
Status : Requested
The Prescription Request is triggered when a HCP clicks on the ‘prescribe’-button. Each Telemonitoring session will initially be created in the status “Requested”.
Status : Accepted
The first thing you need to inform the Telemonitoring HUB of is if you accepted the Telemonitoring Prescription Request. Doing so is done through a PUT request to the Telemonitoring HUB. Changing the status of a Telemonitoring Session to “Accepted” is only possible in case the current status of the session is “requested”.
PUT : https://api.telemonitoring-prescription.com/prescription
HEADERS : { Authorization : access_token }
BODY :
{
telemonitoringId: 'xxx',
status : 'accepted',
providerContext : '<extra provider context>',
carepath : {id : 'hl7-be/...', version : 'x'}
}Note that you can add a providerContext. This can be used if the Telemonitoring Provider wants to add extra context to the HUB, which could be relevant for the EHR.
Status : In-Progress
The status ‘in-progress’ can be sent by the Telemonitoring Provider to inform the EHR the Telemonitoring Session is ongoing and measurements or data relevant to the Telemonitoring Session is or can become available. Changing the status of a Telemonitoring Session to “In-Progress” is only possible in case the current status of the session is “Accepted”.
PUT : https://api.telemonitoring-prescription.com/prescription
HEADERS : { Authorization : access_token }
BODY :
{
telemonitoringId: 'xxx',
status : 'in-progress',
providerContext : '<extra provider context>',
carepath : {id : 'hl7-be/...', version : 'x'}
attachments : [...]
}Note that in the status 'in-progress', attachments can be defined. We cover attachments in a separate section.
Status : Cancelled
“Cancelled” is a status if the HCP decided to cancel a Telemonitoring Session. This is done by the cancel action. Changing the status of a Telemonitoring Session to “Cancelled” is only possible in case the current status of the session is “Requested” or “Accepted”.
Note, that for most Telemonitoring Sessions a cancel can only happen if there was no data measured and only if the Telemonitoring Provider supports the ‘cancel’ action.
PUT : https://api.telemonitoring-prescription.com/prescription
HEADERS : { Authorization : access_token }
BODY :
{
telemonitoringId: 'xxx',
status : 'cancelled',
carepath : {id : 'hl7-be/...', version : 'x'}
}Status : Completed
When the Telemonitoring Session has ended a status update to “Completed” needs to happen. The EHR is in that way informed that no further data will become available on that specific telemonitoring ID. Changing the status of a Telemonitoring Session to “Completed” is only possible in case the current status of the session is “Accepted” or “In-Progress”.
PUT : https://api.telemonitoring-prescription.com/prescription
HEADERS : { Authorization : access_token }
BODY :
{
telemonitoringId: 'xxx',
status : 'completed'
providerContext : '<extra provider context>',
carepath : {id : 'hl7-be/...', version : 'x'}
attachments : [...]
}Attachments
The Telemonitoring HUB can receive 3 types of data and make those available to the EHR.
Properties:
| Name | Description |
|---|---|
| id | Unique id of the attachment |
| name | Optional name of the attachment |
| etag | Unique identifier (optional) |
| contentMD5 | MD5 hash of the content of the attachment. This allows the receiver to verify if the content was changed by a 3th party or not. |
| contentLength | Bytesize of the content |
| lastModified | Timestamp of when the content was last modified |
| contentLanguage | An attachment could be made in a specific language, this contentLanguage can help the receiver to select the right attachment |
| uri | The URL for the attachment |
| headers | Custom headers which need to be set by the receiver when fetching the attachment |
Type 1 : PDF
The PDF gives an overview of the Telemonitoring Session in a human readable format. This can be shared with the health hubs. Every PDF has a unique ID, which makes it possible for the EHR to know if an update to the same file occured. If you share multiple languages, you should add the contentLanguage attribute.
The Telemonitoring HUB does not import or read data in any way. The data remains on the side of the Telemonitoring Provider and it is up to the EHR to download the data. That means the HUB will only share metadata on the PDF.
Example of a PDF document :
{
"id":"pdf",
"name": "Telemonitoring Report",
"etag":"f2fd2ddd34eebc9d039f5e693b95a61c",
"contentMD5":"f2fd2ddd34eebc9d039f5e693b95a61c",
"contentLength":255917,
"contentType":"application/pdf",
"lastModified":"2024-09-30T07:44:17.335Z",
"contentLanguage":"nl",
"uri":"https://xxx/pdf?token=0ba1b31c",
"headers": {
"X-Custom-Header": "HeaderValue"
}
}It’s highly recommended as a Telemonitoring Provider to add MD5 hash and content Length to guarantee there is no data loss or corruption during download of the file by the EHR.
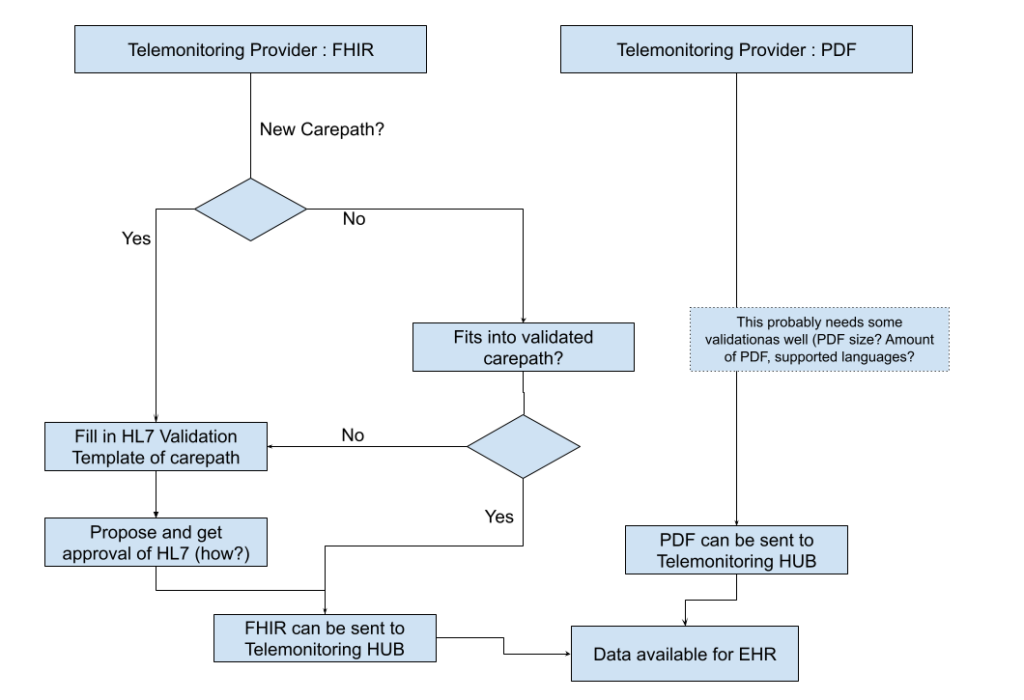
Type 2 : FHIR
Next to PDF, all carepath data that is sent through the Telemonitoring HUB requires a structured FHIR format as well so parsing, visualisation and re-use can be guaranteed. The FHIR format and definition is going through a fixed process, which you can see in the flow chart below.
Example of the FHIR structure
{
"id": "summary",
"name": "Patient Observation"
"contentType": "application/fhir+json",
"contentMD5": "YWIzZGVmNA==",
"contentLength": 120,
"lastModified": "2023-09-02T12:30:00.000-05:00",
"etag": "\"12345abc\"",
"uri": "https://example.com/resource1",
"headers": {
"X-Custom-Header": "HeaderValue"
}
}Type 3 : Dashboard
The final Type is required when visualisation is needed and done by the Telemonitoring Provider. This can be the case by specialized dashboard requirements (for example a neurologists dashboard to monitor and view multi modal signals). In this case a URI is shared that can be included and i-Framed by the EHR.
{
"id": "customId2",
"name": "Patient dashboard
"contentType": "x-tm-dashboard",
"uri": "https://example.com/dashboard",
"headers": {
"X-Dashboard-Header": "DashboardValue"
}
}Securing your data
As the Telemonitoring HUB acts as a gateway for metadata, but doesn’t store data the EHR needs to get data from the Telemonitoring Provider in way that it is safe for the Telemonitoring Provider to not expose this data. There are several ways of doing this and as a Telemonitoring Provider you are free to choose your way of working. Hereby some ways we’ve seen that might work for you.
Obscuring the URI :
This makes the URI impossible to guess, which guarantees that only the EHR can actually read this information.
Adding a prescriber specific token to the URI :
Adding a Token enables you to know what prescriber you’ve sent the data to and validate the correctness of the token. This gives you more control and information versus obscuring the URI.
Limiting in time (signed URI or temporary token) :
This makes the availability of the URI temporary and limits the security risk drastically.
Limiting in requests :
This guarantees a read only-once and so reduces the security risk.
Adding extra headers in the metadata of the HUB :
This URI requires extra authentication that needs to be added by the EHR before downloading. This functionality is currently not supported by the Telemonitoring Portal (so downloading of files with extra authentication will not work with the Telemonitoring Portal)
As an extra security measure some EHR’s will also use white-listing on DNS level and so will require the DNS where you store data on upfront. This will be requested by the Telemonitoring HUB during activation
Attachment Limitations
- There is currently a soft limit of 10 attachments
- There can be multiple FHIR, PDF and Dashboard URI’s available for a Telemonitoring Prescription.
- Every FHIR, PDF and Dashboard are identified by a unique ID defined by the Telemonitoring Provider.
- Every attachment should be made available. If it is out of the array in the webhook, the EHR can mark it as deleted.
Supported Actions
If supported by the Telemonitoring Provider and the EHR, an HCP can trigger actions towards the Telemonitoring Provider. Current supported actions by the Telemonitoring Prescription Portal are stop and cancel.
When the HCP triggers such an action, the Telemonitoring Prescription Portal will trigger the Telemonitoring Provider via the given Action URI:
POST : Action URI webhook
HEADERS : { headers as defined by the Provider }
BODY :
{
telemonitoringId: 'xxx',
prescriber: {
id: '...'
},
action: 'stop' or 'cancel'
}It is up to the Telemonitoring Provider to adjust the status of the Telemonitoring Session according to your business rules and update the Telemonitoring HUB of the status change as described in the section on Status Updates.
I want to get started!
Are you ready to get going and want to get integrated into the Telemonitoring Portal and HUB?
Great! When you’ve implemented the Context and Outcome integration like described above we just need you to send us a bit of information and we will configure you as a Telemonitoring Provider.
What information do we need?
| Name | Telemonitoring Provider Application Name |
| Provider | Telemonitoring Provider Company Name |
| Description | Description available to the HCP |
| Fields | A list of fields (of the available fields which you can find at the top of this page) that you as a provider would like to receive. |
| Supported Actions | [‘stop’, ‘cancel’] : do you support one of these action items? |
| Headers | What headers do you expect the Telemonitoring HUB to include when requesting you? |
| Prescriber specific Headers | What (custom) headers can be filled in by the hospital when configuring / activating you in the portal? |
| URI | What is the URI the HUB can POST to when triggering a new Telemonitoring Prescription. The Telemonitoring Hub also supports Providers who would have a unique URL per Prescriber. |
| Action URI | What is the URI the HUB can POST to when triggering a new Telemonitoring Action |
Once we got this information we’ll set you up as soon as possible and activate an environment for you where you can test the whole flow. After that we can set you up in production.