What is TMP?
Our Mission
Transmural Platform (TMP) exists to accelerate the transition towards transmural care.
To keep high quality healthcare in a landscape with fewer nurses, more chronic disease, and limited hospital capacity, we need to make this shift faster. Today, progress is often slow for understandable reasons, reimbursement frameworks take time to adapt, the sector is highly regulated, and real organisational change is required.
TMP starts at the foundation. We make sure the systems can speak with each other by solving a fundamental building block, data interoperability.
This enables compliant Transmural Data Providers to connect with hospital caregivers, so care pathways can evolve and outcomes can be integrated into clinical workflows.
A hospital without integration
Without standardized integration, telemonitoring and transmural data often live outside the hospital workflow.
The result is not just technical complexity, it directly affects usability, safety, and scalability.
What typically happens
- No Single Sign-On
Extra accounts and logins create friction and reduce security, especially at scale. - No workflow integration
Requests, follow-up, and interpretation happen outside the normal clinical flow. - Separate applications next to the EHR
Clinicians need to switch tools constantly, context is lost and adoption suffers. - Shadow IT and unmanaged workarounds
Local spreadsheets, emails, shared inboxes, and ad-hoc portals appear to fill the gaps. - Manual data transfer
Copying values between systems or re-entering information is time-consuming and error-prone. - Federated data across multiple systems
Data ends up spread across provider platforms and separate tools, often without clear hospital-level oversight. - No structured and actionable data
Results arrive as PDFs, screenshots, or unstructured text, making it hard to trend, alert, or act. - Manual errors and inconsistency
Copy-paste mistakes, missing context, and different formats reduce clinical reliability. - No standardisation
Each provider integration is different, which increases cost and slows down rollout across care pathways.
Why not integrate it yourself?
Many hospitals and EHR vendors can integrate directly with individual providers. It works, until it needs to scale.
The reality at scale
- One integration becomes many
Each provider has different data models, security approaches, and operational processes.
What starts as one project quickly becomes a portfolio of integrations to build, test, and maintain. - Maintenance never stops
Providers evolve, care pathways change, regulations and security requirements tighten, and EHR upgrades happen.
The long-term cost is in lifecycle management, not the first go-live. - Security and compliance need consistency
Every integration requires vendor assessment, contract alignment, DPIA-style evaluations, access control, auditing, and incident processes.
Doing this repeatedly for every provider is heavy and error-prone. - You still need a return flow that is usable
Without standardisation, results arrive in different formats and levels of structure, making it hard to build reliable clinical workflows, dashboards, and alerts inside the EHR. - Single Sign-On and identity become fragmented
Separate accounts, separate portals, separate access reviews. This reduces usability and increases security risk. - Hard to stay neutral and future-proof
Bilateral integrations can lock you into specific vendors or approaches, making it harder to add new (or replace old) providers or expand across care pathways.
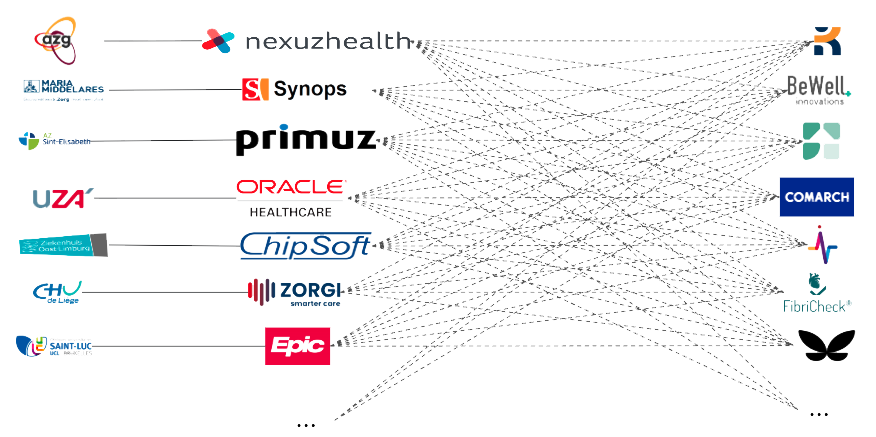
This image illustrates the many to many problem that exists when you have one-to-one integrations between hospitals – EHR’s and Data Providers.
The cost is huge from hospital, EHR and Data Provider point of view.
Integration through TMP
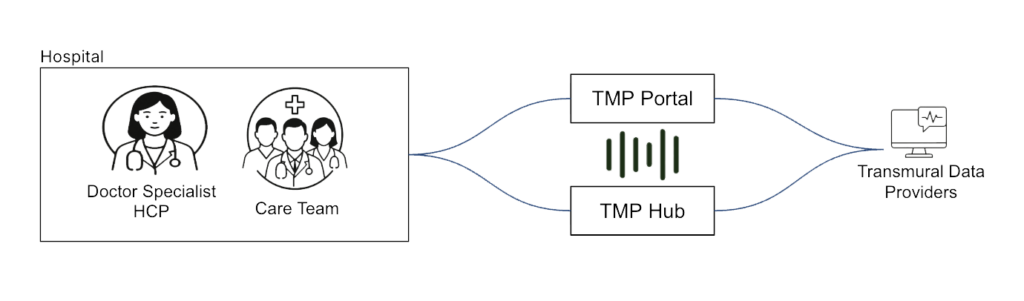
TMP provides a standardised request and return flow for transmural data.
Hospitals use the TMP Portal to request a compliant Transmural Data Provider and securely share the required context.
Providers return results through the TMP Hub, where outcomes are delivered back to hospitals and EHR systems in a consistent, structured way.
TMP fundamentals
TMP Portal
The view for hospitals and healthcare professionals, enabling provider selection, context sharing, and operational transparency.
Fully integrated into their EHR.
TMP Hub
The gateway that returns structured results to hospitals and EHRs, aligned with interoperable HL7 standards.
FAIR and FIHR
Why this matters
- Network effect
As more hospitals and more Transmural Data Providers connect, integration becomes easier for everyone, integrate once and scale across the network. - Integration with a click of a button
Hospitals can request a provider and start the process without a custom project for every new connection. - Trusted and transparent provider onboarding
Full visibility on valid providers, including care paths, privacy posture, security, and clear data flows. - Structured data, standardised format
Results are returned in a structured way aligned with HL7 and modern interoperability practices, not tied to a single region, vendor, or country. - Adapters to EHR systems
TMP reduces EHR implementation effort by providing reusable adapters and a consistent integration approach, making it worth it for both hospitals and EHR vendors. - Standardised workflows across care paths
A consistent request and return workflow across multiple clinical pathways, reducing training and operational complexity. - Clarity for hospital management
Clear data flows and governance, supporting security reviews, operational oversight, and predictable lifecycle management. - Hooks into existing national infrastructure
TMP can connect with country-specific building blocks where needed, without losing the benefits of a shared European interoperability approach.